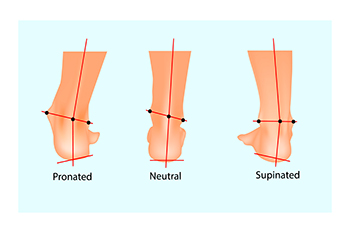
Understanding supination, also called underpronation, is essential for maintaining foot health. Supination occurs when your weight rolls onto the outer edges of the feet during movement. It is often the result of inherited structural issues or muscle weakness. Unfortunately, excessive supination can lead to various problems, including back and hip pain, knee stress, ankle injuries, and plantar fasciitis. Supination can also cause tension in different parts of the body over time, increasing the risk of injuries. Seeking medical help from a podiatrist for a gait analysis is advisable if you suspect supination, or are experiencing unexplained lower body pain. Treatment typically involves corrective measures to address foot alignment and prevent future injuries. This may include selecting appropriate footwear with extra cushioning and room in the toes, using custom-made orthotic insoles, and performing strength and stretching exercises as suggested by a podiatrist. Proper care and intervention can alleviate discomfort and prevent complications associated with supination, ensuring optimal mobility and well-being. If you believe you have pain that results from supination, it is suggested that you schedule an appointment with a podiatrist.
If you have any concerns about your feet, contact one of our podiatrists from Centers for Foot & Ankle Care. Our doctors can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact one of our offices located in Merrillville, Portage, Michigan City/LaPorte, and Schererville, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
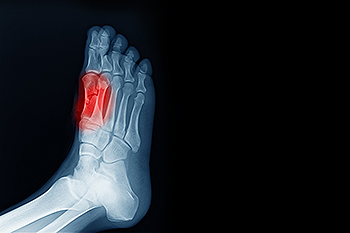 Sesamoiditis is an inflammation of the sesamoid bones, two tiny bones beneath the big toe joint. These bones are embedded within the tendons that allow the big toe to move. Sesamoiditis typically occurs from overuse or repetitive stress, making it common among athletes and dancers. Symptoms of sesamoiditis include pain in the ball of the foot, especially when walking or running, and swelling or bruising in the area around the big toe. The pain might worsen when the big toe is used, such as when pushing off to jump or take a step. Bending and straightening the big toe may also become difficult. If you have a painful big toe or ball of the foot, it is suggested that you consult a podiatrist for a proper diagnosis and treatment plan.
Sesamoiditis is an inflammation of the sesamoid bones, two tiny bones beneath the big toe joint. These bones are embedded within the tendons that allow the big toe to move. Sesamoiditis typically occurs from overuse or repetitive stress, making it common among athletes and dancers. Symptoms of sesamoiditis include pain in the ball of the foot, especially when walking or running, and swelling or bruising in the area around the big toe. The pain might worsen when the big toe is used, such as when pushing off to jump or take a step. Bending and straightening the big toe may also become difficult. If you have a painful big toe or ball of the foot, it is suggested that you consult a podiatrist for a proper diagnosis and treatment plan.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact one of our podiatrists of Centers for Foot & Ankle Care. Our doctors will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact one of our offices located in Merrillville, Portage, Michigan City/LaPorte, and Schererville, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

First and foremost, wearing ill-fitting shoes can lead to a myriad of injuries. Whether they are too tight, too loose, or simply not designed for the activity you are engaging in, improper footwear can place undue stress on your feet, ankles, lower legs, and joints, increasing your risk of pain and injury. From common issues like shin splints and ingrown nails to more severe problems such as bunions and postural misalignments, the repercussions of wearing the wrong shoes can be far-reaching and debilitating, potentially limiting your ability to engage in physical activity altogether. Furthermore, wearing the wrong shoes can worsen existing conditions, such as arthritis, making daily activities more challenging and uncomfortable. Plus, when your shoes fail to support your natural gait or foot structure, it can lead to overpronation, underpronation, or other biomechanical issues, placing added strain on your joints and increasing your risk of injury. If your feet are painful after performing certain activities or from wearing certain shoes, it is suggested that you schedule an appointment with a podiatrist to determine whether your footwear may need to be changed.
Finding a properly-fitting shoe is important in reducing injuries and preventing foot problems. For more information about treatment, contact one of our podiatrists from Centers for Foot & Ankle Care. Our doctors will treat your foot and ankle needs.
Proper Shoe Fitting
A common concern when it comes to foot health, having properly fitted shoes can help prevent injuries to the foot. Out feet affect our posture and gait, which in turn affects the biomechanics and overall bodily structure. With 33 joints, 26 bones, and over 100 ligaments, the potential for serious injury is much greater than one realizes. Although the feet cease growth in adulthood, they still change shape as they mature. Here are some factors to consider when it comes to investing in proper fitting shoes:
- Be sure the shoes fit correctly right away
- Ensure the ball of your foot fits comfortably in the widest portion of the shoes
- Even though they may look fashionable, improper fitting shoes can either create adverse conditions or exacerbate existing ones you may already have
- Walk along a carpeted surface to ensure the shoes comfortably fit during normal activity
Keeping in mind how shoes fit the biomechanics of your body, properly-fitting shoes are vitally important. Fortunately, it is not difficult to acquire footwear that fits correctly. Be sure to wear shoes that support the overall structure of your body. Do your feet a favor and invest in several pairs of well-fitted shoes today.
If you have any questions please feel free to contact one of our offices located in Merrillville, Portage, Michigan City/LaPorte, and Schererville, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.