
Different Types of Bunions and Treatments

A bunion is a bony bump that forms when the big toe joint shifts out of alignment, often due to genetics, wearing improper footwear, flat feet, or arthritis. Over time, the joint becomes swollen, painful, and stiff, making walking uncomfortable. There are different types of bunions. The most common is the classic bunion, which develops on the inside of the foot at the base of the big toe. A tailor’s bunion, or bunionette, forms on the outside at the base of the little toe. A dorsal bunion occurs on the top of the big toe joint, often limiting movement and making shoe wear painful. Treatment varies based on severity. Wider shoes, padding, orthotics, and toe exercises can help, and severe cases may require injections or surgery. Since bunions worsen over time, it is suggested that you see a podiatrist for early intervention and to prevent complications.
If you are suffering from bunion pain, contact one of our podiatrists of Centers for Foot & Ankle Care. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
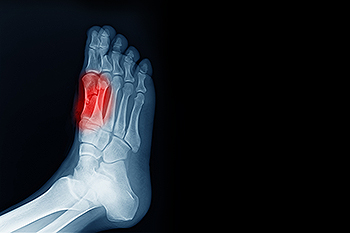
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Merrillville, Portage, Michigan City/LaPorte, and Schererville, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
Types of Flat Feet

Flat feet, also known as fallen arches, occur when the arch of the foot collapses, causing the entire foot to make contact with the ground. There are two types, which are flexible and rigid. Flexible flat feet are more common and typically cause discomfort after standing or walking for long periods. Rigid flat feet, which are less flexible, can cause significant pain, especially when walking or running. Symptoms include pain in the arch, heel, or knees, and you may notice that your feet appear to roll inward. The causes of flat feet include genetics, injury, or weakened tendons. A podiatrist can help by evaluating your foot structure and offering treatments like custom orthotics to support the arch, exercises to strengthen the foot, and surgery for more severe cases. If you have flat feet, it is suggested that you schedule an appointment with a podiatrist to get the right treatment and improve comfort.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from Centers for Foot & Ankle Care. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact one of our offices located in Merrillville, Portage, Michigan City/LaPorte, and Schererville, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flat Feet
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.
Stretches That Help With Plantar Fasciitis

Plantar fasciitis results when the thick band of tissue along the sole of the foot becomes inflamed, leading to heel pain and stiffness. Stretching exercises can help relieve this discomfort by improving flexibility and reducing strain on the plantar fascia. A calf stretch can be done by placing both hands against a wall, stepping one foot back, and pressing the heel into the ground while bending the front knee. Holding this position helps lengthen the Achilles tendon and ease tension in the foot. A stair stretch involves standing on a step with the heels hanging off the edge, then gently lowering them to stretch the back of the foot and ankle. A seated foot stretch can be performed by grasping the toes and pulling them toward the shin, which targets the arch directly. Using a towel or resistance band around the toes while pulling upward can also stretch the bottom of the foot. If you are experiencing pain in the heel or on the bottom of your foot, it may be a sign of plantar fasciitis, and it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment options.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Centers for Foot & Ankle Care. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact one of our offices located in Merrillville, Portage, Michigan City/LaPorte, and Schererville, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Definition of a Heel Spur

Heel spurs are bony growths that can form on the underside of the heel bone, often associated with plantar fasciitis. These spurs develop over time as a result of repetitive stress or tension on the foot. The primary cause is the strain placed on the plantar fascia, a thick band of tissue that connects the heel to the toes. As this tissue is repeatedly stretched or stressed, calcium deposits may accumulate, leading to the formation of a heel spur. Common symptoms include sharp pain in the heel, particularly when walking or standing after rest. Swelling and tenderness surrounding the heel area may also occur. Although heel spurs are often painless, they can cause significant discomfort and restrict normal movement if left untreated. If you have heel pain, it is suggested that you contact a podiatrist who can accurately diagnose a heel spur, and offer appropriate relief and treatment solutions.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from Centers for Foot & Ankle Care. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact one of our offices located in Merrillville, Portage, Michigan City/LaPorte, and Schererville, IN . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
What Is Sesamoiditis?
Sesamoiditis is a painful condition that affects two small sesamoid bones located under the big toe joint. It occurs when these bones become irritated or inflamed, usually due to overuse or repetitive pressure from high-impact activities like running or jumping. Symptoms include pain at the base of the big toe, swelling, and tenderness, especially when bearing weight or pushing off during walking or running. The pain from sesamoiditis can feel sharp or throbbing, and it often worsens with activity. Rest and anti-inflammatory medications are common initial treatments. Wearing cushioned footwear or using custom orthotics to reduce pressure on the affected area can also help. In more severe cases, your podiatrist may recommend corticosteroid injections. This type of doctor specializes in diagnosing and treating conditions like sesamoiditis, helping to reduce pain and prevent further damage. If you are experiencing pain near the base of your big toe, it is suggested that you schedule an appointment with a podiatrist for a tailored treatment plan.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact one of our podiatrists of Centers for Foot & Ankle Care. Our doctors will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact one of our offices located in Merrillville, Portage, Michigan City/LaPorte, and Schererville, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.







